Anemia is strictly defined as a decrease in red blood cell (RBC) mass. The function of the RBC is to deliver oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs. This is accomplished by using hemoglobin (Hb), a tetramer protein composed of heme and globin. Anemia impairs the body’s ability for gas exchange by decreasing the number of RBCs transporting oxygen and carbon dioxide.
CAUSES
Although many parts of the body help make red blood cells, most of the work is done in the bone marrow. Bone marrow is the soft tissue in the center of bones that helps form all blood cells.Most often healthy red blood cells last between 90 and 120 days. Parts of your body then remove old blood cells. A hormone called erythropoietin (epo) made in your kidneys signals your bone marrow to make more red blood cells.
Hemoglobin is the oxygen-carrying protein inside red blood cells. It gives red blood cells their red color. People with anemia do not have enough hemoglobin.
The body needs certain vitamins,
minerals, and nutrients to make enough red blood cells. Iron, vitamin B12, and folic acid are three of the most important ones. The body may not have enough of these nutrients because:
- Changes in the lining of the stomach or intestines affect how well nutrients are absorbed (for example, celiac disease)
- Poor diet
- Slow blood loss (for example, from heavy menstrual periods or stomach ulcers)
- Surgery that removes part of the stomach or intestines
- Certain medications
- Destruction of red blood cells earlier than normal (which may be caused by immune system problems)
- Long-term (chronic) diseases such as chronic kidney disease, cancer, ulcerative colitis, or rheumatoid arthritis
- Some forms of anemia, such as thalassemia or sickle cell anemia, which can be inherited
- Pregnancy
- Problems with bone marrow such as lymphoma, leukemia, multiple myeloma, or aplastic anemia.
SYMPTOMS
You may have no symptoms if the anemia is mild. If the problem develops slowly, symptoms that may occur first include:- Feeling grumpy
- Feeling weak or tired more often than usual, or with exercise
- Headaches
- Problems concentrating or thinking
- Blue color to the whites of the eyes
- Brittle nails
- Light-headedness when you stand up
- Pale skin color
- Shortness of breath
- Sore tongue
EXAMS AND TESTS
The doctor will perform a physical examination, and may find:- Heart murmur
- Low blood pressure, especially when you stand up
- Pale skin
- Rapid heart rate
Blood tests used to diagnose some common types of anemia may include:
- Blood levels of iron, vitamin B12, folic acid, and other vitamins and minerals
- Red blood count and hemoglobin level
- Reticulocyte count
TREATMENT
Treatment should be directed at the cause of the anemia, and may include:- Blood transfusions
- Corticosteroids or other medicines that suppress the immune system
- Erythropoietin, a medicine that helps your bone marrow make more blood cells
- Supplements of iron, vitamin B12, folic acid, or other vitamins and minerals
Other types of anemia include:
1)Vitamin B12 deficiency=
Vitamin B12 deficiency anemia is a low red blood cell count due to a lack of vitamin B12. Anemiais a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
CAUSES:
Your body needs vitamin B12 to make red blood cells. In order to provide vitamin B12 to your cells:
You must eat plenty of foods that contain vitamin B12, such as meat, poultry, shellfish, eggs, and dairy products.
Your body must absorb enough vitamin B12. A special protein, called intrinsic factor, helps your body do this. This protein is released by cells in the stomach.
A lack of vitamin B12 may be due to dietary factors, including:
Eating a vegetarian diet
Poor diet in infants
Poor nutrition during pregnancy
Certain health conditions can make it difficult for your body to absorb enough vitamin B12. They include:
Chronic alcoholism
Crohn's disease, celiac disease, infection with the fish tapeworm, or other problems that make it difficult for your body to digest foods
Pernicious anemia, a type of vitamin B12 anemia that occurs when your body destroys cells that make intrinsic factor
Surgeries that remove certain parts of your stomach or small intestine, such as some weight-loss surgeries
Taking antacids and other heartburn medicines for a long period of time.
Symptoms
You may not have symptoms. Symptoms may be mild.Symptoms can include:
- Diarrhea or constipation
- Fatigue, lack of energy, or light-headedness when standing up or with exertion
- Loss of appetite
- Pale skin
- Problems concentrating
- Shortness of breath, mostly during exercise
- Swollen, red tongue or bleeding gums
- Confusion or change in mental status (dementia) in severe cases
- Depression
- Loss of balance
- Numbness and tingling of hands and feet.
Exams and Tests
The doctor or nurse will perform a physical exam. This may reveal problems with your reflexes.Tests that may be done include:
- Complete blood count (CBC)
- Reticulocyte count
- LDH level
- Vitamin B12 level
Other procedures that may be done include:
- Esophagogastroduodenoscopy (EGD) to examine the stomach
- Enteroscopy to examine the small intestine
- Bone marrow biopsy if the diagnosis is not clear.
Treatment
Treatment depends on the cause of B12 deficiency anemia. For treatment of anemia due to a lack of intrinsic factor, see: Pernicious anemiaThe goal of treatment is to increase your vitamin B12 levels.
- Treatment may include a shot of vitamin B12 once a month. Persons with severely low levels of B12 may need more shots in the beginning. You may need shots every month for the rest of your life.
- Some patients may also need to take vitamin B12 supplements by mouth. For some people, high-dose vitamin B12 tablets taken by mouth work well, and shots are not needed.
Treatment may no longer be needed after Crohn's disease, celiac disease, or alcoholism is properly treated.
Your doctor or nurse will also recommend eating a well-balanced diet.Prevention
You can prevent anemia caused by a lack of vitamin B12 by following a well-balanced diet.Shots of vitamin B12 can prevent anemia after surgeries known to cause vitamin B12 deficiency.
Early diagnosis and prompt treatment can reduce or prevent complications related to low vitamin B12 levels.
2)Folate-Deficiency Anemia=
Folate-deficiency anemia is a decrease in red blood cells (anemia) due to a lack of folate. Folate is a type of B vitamin. It is also called folic acid.
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
In folate-deficiency anemia, the red blood cells are abnormally large. Such cells are called megalocytes. They are also called megaloblasts. They are seen in the bone marrow. This is why this anemia is also called megaloblastic anemia.
Causes of this type of anemia include:
You may receive folic acid supplements, taken by mouth or given through a vein. If you have low folate levels because of a problem with your intestines, you make need treatment for the rest of your life.
Diet changes can help boost your folate level. Eat more green, leafy vegetables and citrus fruits.
Experts recommend that women take 400 micrograms (mcg) of folic acid every day before you get pregnant through the first 3 months of pregnancy.
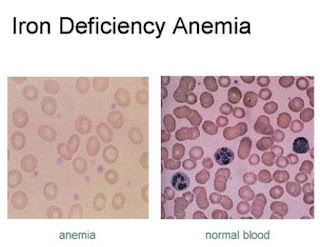
When your body does not have enough iron, it will make fewer red blood cells or red blood cells that are too small. This is called iron deficiency anemia.
Red blood cells bring oxygen to the body's tissues. Healthy red blood cells are made in your bone marrow. Red blood cells circulate through your body for 3 to 4 months. Parts of your body like your spleen remove old blood cells.
Iron is a key part of red blood cells. Without iron, the blood cannot carry oxygen effectively. Your body normally gets iron through your diet. It also reuses iron from old red blood cells.
You get iron deficiency anemia when your body's iron stores run low. This can occur because:
Most of the time, symptoms are mild at first and develop slowly. Symptoms may include:
Treatment may include taking iron supplements and eating iron-rich foods.
Iron supplements (most often ferrous sulfate) are needed to build up the iron stores in your body. Most of the time, your doctor or nurse will measure your iron levels before starting supplements.
If you cannot take iron by mouth, you may need to take it through a vein (intravenous) or by an injection into the muscle.
Pregnant and breastfeeding women will need to take extra iron because they often cannot get enough iron from their normal diets.
Your hematocrit should return to normal after 2 months of iron therapy. You will need to keep taking iron for another 6 - 12 months to replace the body's iron stores in the bone marrow.
Iron-rich foods include:
Anemia of chronic disease is anemia that is found in people with certain long-term (chronic) medical conditions.
Conditions that can lead to anemia of chronic disease include:
If they occur, smptoms may include:
Because anemia may be the first symptom of a serious illness, determining its cause is very important.
Tests that may be done to diagnose anemia or rule out other causes include:
The condition is rarely severe enough to need a blood transfusion.
Iron supplements may sometimes be used, but only for patients whose iron levels are low. Taking iron pills when your body does not need it can lead to serious medical problems. Always talk with your health care provider first.
For some conditions, such as chronic kidney disease, medicine called erythropoietin may be given. It stimulates your bone marrow to make more red blood cells.
Immune hemolytic anemia occurs when the immune system mistakenly sees your own red blood cells as foreign substances. Antibodies then develop against the red blood cells. These antibodies attack the red blood cells and cause them to break down too early.
The body may also destroy red blood cells because of:
These tests can identify the type of hemolytic anemia:
Aplastic anemia can also be caused by certain medical conditions such as pregnancy or lupus. Exposure to certain toxins or medicines, including chemotherapy, can also lead to aplastic anemia.
Low red cell count (anemia) can cause:
Low platelet count (thrombocytopenia) can result in bleeding. Symptoms include:
Blood tests will show:
If blood counts become lower, patients receive extra blood and platelets through transfusions. Over time, transfusions may stop working, resulting in very low blood cell counts. This is a life-threatening condition.
Bone marrow transplant or stem cell transplant may be recommended for patients under age 40. This treatment works best when the donor is a fully-matched brother or sister. This is called a matched sibling donor.
Older patients and those who do not have a matched sibling donor are given medicines to suppress the immune system. These medicines may allow the bone marrow to once again make healthy blood cells. But the disease may return (relapse). A bone marrow transplant with an unrelated donor may be tried if these medicines do not help or if the disease comes back after getting better.
A special protein, called intrinsic factor, helps your intestines absorb vitamin B12. This protein is released by cells in the stomach. When the stomach does not make enough intrinsic factor, the intestine cannot properly absorb vitamin B12.
Common causes of pernicious anemia include:
In adults, symptoms of pernicious anemia are usually not seen until after age 30. The average age of diagnosis is age 60.
You are more likely to get this disease if you:
They can include:
Pernicious anemia may also affect the results of the following tests:
Sickle cell disease is much more common in people of African and Mediterranean descent. It is also seen in people from South and Central America, the Caribbean, and the Middle East.
Almost all people with sickle cell anemia have painful episodes called crises. These can last from hours to days. Crises can cause pain in the lower back, leg, joints, and chest.
Some people have one episode every few years. Others have many episodes each year. The crises can be severe enough to require a hospital stay.
When the anemia becomes more severe, symptoms may include:
Younger children with sickle cell anemia have attacks of abdominal pain.
The following symptoms may occur because small blood vessels become blocked by the abnormal cells:
People with this condition should take folic acid supplements. Folic acid helps make new red blood cells.
Treatment for a sickle cell crisis includes:
People with sickle cell disease should have the following vaccinations to lower the risk of infection:
There are two main types of thalassemia:
Beta thalassemias occur most often in persons of Mediterranean origin. To a lesser extent, Chinese, other Asians, and African Americans can be affected.
There are many forms of thalassemia. Each type has many different subtypes. Both alpha and beta thalassemia include the following two forms:
Thalassemia minor occurs if you receive the faulty gene from only one parent. Persons with this form of the disorder are carriers of the disease. Most of the time, they do not have symptoms.
Beta thalassemia major is also called Cooley's anemia.
Risk factors for thalassemia include:
Children born with thalessemia major (Cooley's anemia) are normal at birth, but develop severe anemia during the first year of life.
Other symptoms can include:
If you receive blood transfusions, you should not take iron supplements. Doing so can cause a high amount of iron to build up in the body, which can be harmful.
Persons who receive a lot of blood transfusions need a treatment called chelation therapy. This is done to remove excess iron from the body.
A bone marrow transplant may help treat the disease in some patients, especially children.
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
Causes
Folate (folic acid) is needed for red blood cells to form and grow. You can get folate by eating green leafy vegetables and liver. However, your body does not store folate in large amounts. So, you need to eat plenty of folate-rich foods to maintain normal levels of this vitamin.In folate-deficiency anemia, the red blood cells are abnormally large. Such cells are called megalocytes. They are also called megaloblasts. They are seen in the bone marrow. This is why this anemia is also called megaloblastic anemia.
Causes of this type of anemia include:
- Too little folic acid in your diet
- Hemolytic anemia
- Long-term alcoholism
- Use of certain medications (such as phenytoin [Dilantin], methotrexate, sulfasalazine, triamterene, pyrimethamine, trimethoprim-sulfamethoxazole, and barbiturates)
- Alcoholism
- Eating overcooked food
- Poor diet (often seen in the poor, the elderly, and people who do not eat fresh fruits or vegetables)
- Pregnancy
Symptoms
Exams and Tests
The doctor or nurse will perform a physical exam. Tests that may be done include:- Complete blood count (CBC)
- Red blood cell folate level
Treatment
The goal is to identify and treat the cause of the folate deficiency.You may receive folic acid supplements, taken by mouth or given through a vein. If you have low folate levels because of a problem with your intestines, you make need treatment for the rest of your life.
Diet changes can help boost your folate level. Eat more green, leafy vegetables and citrus fruits.
Prevention
Eating plenty of folate rich foods can help prevent this condition.Experts recommend that women take 400 micrograms (mcg) of folic acid every day before you get pregnant through the first 3 months of pregnancy.
3)Iron Deficiency Anemia=
Anemia is a condition in which the body does not have enough healthy red blood cells. Iron helps make red blood cells.When your body does not have enough iron, it will make fewer red blood cells or red blood cells that are too small. This is called iron deficiency anemia.
Causes
Iron deficiency anemia is the most common form of anemia.Red blood cells bring oxygen to the body's tissues. Healthy red blood cells are made in your bone marrow. Red blood cells circulate through your body for 3 to 4 months. Parts of your body like your spleen remove old blood cells.
Iron is a key part of red blood cells. Without iron, the blood cannot carry oxygen effectively. Your body normally gets iron through your diet. It also reuses iron from old red blood cells.
You get iron deficiency anemia when your body's iron stores run low. This can occur because:
- You lose more blood cells and iron than your body can replace
- Your body does not do a good job of absorbing iron
- Your body is able to absorb iron, but you are not eating enough foods that contain iron.
- Your body needs more iron than normal (such as if you are pregnant or breastfeeding)
- Heavy, long, or frequent menstrual periods
- Cancer in the esophagus, stomach, or colon
- Esophageal varices usually from cirrhosis
- The use of aspirin, ibuprofen, or arthritis medicines for a long time, which can cause gastrointestinal bleeding
- Peptic ulcer disease
- Celiac disease
- Crohn's disease
- Gastric bypass surgery
- Taking too many antacids that contain calcium
- You are a strict vegetarian
- You are an older adult and do not eat a full diet.
Symptoms
You may have no symptoms if the anemia is mild.Most of the time, symptoms are mild at first and develop slowly. Symptoms may include:
- Feeling grumpy
- Feeling weak or tired more often than usual, or with exercise
- Headaches
- Problems concentrating or thinking
- Blue color to the whites of the eyes
- Brittle nails
- Light-headedness when you stand up
- Pale skin color
- Shortness of breath
- Sore tongue
- Dark, tar-colored stools or blood
- Heavy menstrual bleeding (women)
- Pain in the upper belly (from ulcers)
- Weight loss (in people with cancer)
TREATMENT
Exams and Tests
To diagnose anemia, your doctor may order these blood tests:- Hematocrit and hemoglobin (red blood cell measures)
- RBC indices
Treatment
Before treatment, you and your health care provider must first search for the cause of your anemia. Next, the reason for iron deficiency needs to be discovered.Treatment may include taking iron supplements and eating iron-rich foods.
Iron supplements (most often ferrous sulfate) are needed to build up the iron stores in your body. Most of the time, your doctor or nurse will measure your iron levels before starting supplements.
If you cannot take iron by mouth, you may need to take it through a vein (intravenous) or by an injection into the muscle.
Pregnant and breastfeeding women will need to take extra iron because they often cannot get enough iron from their normal diets.
Your hematocrit should return to normal after 2 months of iron therapy. You will need to keep taking iron for another 6 - 12 months to replace the body's iron stores in the bone marrow.
Iron-rich foods include:
- Chicken and turkey
- Dried lentils, peas, and beans
- Fish
- Meats (liver is the highest source)
- Peanut butter
- Soybeans
- Whole-grain bread
- Oatmeal
- Raisins, prunes, and apricots
- Spinach, kale, and other greens.
Prevention
A well rounded diet should include enough iron. Red meat, liver, and egg yolks are high sources of iron. Flour, bread, and some cereals are fortified with iron. Take iron supplements if you aren't getting enough iron in your die.4)Anemia of Chronic Disease=
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. There are many types of anemia.Anemia of chronic disease is anemia that is found in people with certain long-term (chronic) medical conditions.
Causes
Anemia is a lower-than-normal number of red blood cells in the blood. Certain chronic infections, inflammatory diseases, and other illnesses can affect the body's ability to produce red blood cells.Conditions that can lead to anemia of chronic disease include:
- Autoimmune disorders, such as Crohn's disease, systemic lupus erythematosus, rheumatoid arthritis, and ulcerative colitis
- Cancer, including lymphoma and Hodgkin's disease
- Chronic kidney disease
- Liver cirrhosis
- Long-term infections, such as bacterial endocarditis, osteomyelitis (bone infection), HIV/AIDS, hepatitis B or hepatitis C.
Symptoms
Anemia of chronic disease is often mild. You may not notice symptoms of anemia.If they occur, smptoms may include:
- Feeling weak or tired
- Headache
- Paleness
- Shortness of breath.
Exams and Tests
The doctor will perform a physical examination.Because anemia may be the first symptom of a serious illness, determining its cause is very important.
Tests that may be done to diagnose anemia or rule out other causes include:
- Hemoglobin level
- Red blood count
- Reticulocyte count
- Serum ferritin
- Serum iron
- Other blood tests.
Treatment
Anemia is often mild enough that it does not need treatment. It will likely get better when the disease that is causing it is treated.The condition is rarely severe enough to need a blood transfusion.
Iron supplements may sometimes be used, but only for patients whose iron levels are low. Taking iron pills when your body does not need it can lead to serious medical problems. Always talk with your health care provider first.
For some conditions, such as chronic kidney disease, medicine called erythropoietin may be given. It stimulates your bone marrow to make more red blood cells.
5)Hemolytic Anemia=
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
Normally, red blood cells last for about 120 days before the body gets rid of them. In hemolytic anemia, red blood cells in the blood are destroyed earlier than normal.
Normally, red blood cells last for about 120 days before the body gets rid of them. In hemolytic anemia, red blood cells in the blood are destroyed earlier than normal.
Causes
Hemolytic anemia occurs when the bone marrow is unable to replace the red blood cells that are being destroyed.Immune hemolytic anemia occurs when the immune system mistakenly sees your own red blood cells as foreign substances. Antibodies then develop against the red blood cells. These antibodies attack the red blood cells and cause them to break down too early.
The body may also destroy red blood cells because of:
- Certain genetic defects that cause the blood cells to take on abnormal shapes (such as sickle cell anemia, thalassemia, and hemolytic anemia due to G6PD deficiency
- Exposure to certain chemicals, drugs, and toxins
- Infections
- Blood clots in small blood vessels
- Transfusion of blood from a donor with a blood type that does not match yours.
Symptoms
You may not have symptoms if the anemia is mild. If the problem develops slowly, the first symptoms may be:- Feeling grumpy
- Feeling weak or tired more often than usual, or with exercise
- Headaches
- Problems concentrating or thinking
- Blue color to the whites of the eyes
- Brittle nails
- Light-headedness when you stand up
- Pale skin color
- Shortness of breath
- Sore tongue
Exams and Tests
A test called a complete blood count (CBC) can help diagnose anemia and offer some hints to the type and cause of the problem. Important parts of the CBC include red blood cell count (RBC), hemoglobin, and hematocrit (HCT).These tests can identify the type of hemolytic anemia:
- Absolute reticulocyte count
- Coombs' test, direct
- Coombs' test, indirect
- Donath-Landsteiner test
- Febrile or cold agglutinins
- Free hemoglobin in the serum or urine
- Hemosiderin in the urine
- Platelet count
- Protein electrophoresis - serum
- Serum haptoglobin levels
- Serum LDH
- Urine and fecal urobilinogen
Treatment
Treatment depends on the type and cause of the hemolytic anemia.- In emergencies, a blood transfusion may be needed.
- For hemolytic anemia caused by an overactive immune system, drugs that suppress the immune system may be used.
- When blood cells are being destroyed at a fast pace, the body may need extra folic acid and iron supplements to replace what is being lost.
6)Aplastic Anemia=
Aplastic anemia is a condition in which the bone marrow does not make enough new blood cells. Bone marrow is the soft, fatty tissue in the center of bones.Causes
Aplastic anemia results from injury to the blood stem cells. These are immature cells in the bone marrow that give rise to all other blood cells types. The injury causes a decrease in the number of every type of blood cell. These cells are the red cells, white cells, and platelets.Aplastic anemia can also be caused by certain medical conditions such as pregnancy or lupus. Exposure to certain toxins or medicines, including chemotherapy, can also lead to aplastic anemia.
Symptoms
Symptoms result from the bone marrow not being able to make new blood cells. Symptoms may be severe from the start or gradually worsen over time.Low red cell count (anemia) can cause:
- Fatigue
- Pallor (paleness)
- Rapid heart rate
- Shortness of breath with exercise
- Weakness
- Lightheadedness upon standing
Low platelet count (thrombocytopenia) can result in bleeding. Symptoms include:
- Bleeding gums
- Easy bruising
- Frequent or severe infections
- Nose bleeds
- Rash--small pinpoint red marks on the skin (petechiae).
Exams and Tests
The health care provider will perform a physical exam.Blood tests will show:
- Low red blood cell count (anemia)
- Low white blood cell count
- Low reticulocyte count (reticulocytes are immature red blood cell)
- Low platelet count
Treatment
Mild cases of aplastic anemia may require no treatment. Symptoms are treated as needed.If blood counts become lower, patients receive extra blood and platelets through transfusions. Over time, transfusions may stop working, resulting in very low blood cell counts. This is a life-threatening condition.
Bone marrow transplant or stem cell transplant may be recommended for patients under age 40. This treatment works best when the donor is a fully-matched brother or sister. This is called a matched sibling donor.
Older patients and those who do not have a matched sibling donor are given medicines to suppress the immune system. These medicines may allow the bone marrow to once again make healthy blood cells. But the disease may return (relapse). A bone marrow transplant with an unrelated donor may be tried if these medicines do not help or if the disease comes back after getting better.
7)Pernicious Anemia=
Pernicious anemia is a decrease in red blood cells that occurs when your intestines cannot properly absorb vitamin B12.Causes
Pernicious anemia is a type of vitamin B12 anemia. The body needs vitamin B12 to make red blood cells. You get this vitamin from eating foods such as meat, poultry, shellfish, eggs, and dairy products.A special protein, called intrinsic factor, helps your intestines absorb vitamin B12. This protein is released by cells in the stomach. When the stomach does not make enough intrinsic factor, the intestine cannot properly absorb vitamin B12.
Common causes of pernicious anemia include:
- Weakened stomach lining (atrophic gastritis)
- An autoimmune condition in which the body's immune system attacks intrinsic factor protein or the cells that make it.
In adults, symptoms of pernicious anemia are usually not seen until after age 30. The average age of diagnosis is age 60.
You are more likely to get this disease if you:
- Scandinavian or Northern European
- Have a family history of the condition
- Addison's disease
- Chronic thyroiditis
- Graves disease
- Hypoparathyroidism
- Hypopituitarism
- Myasthenia gravis
- Secondary amenorrhea
- Type 1 diabetes
- Testicular dysfunction
- Vitiligo.
Symptoms
Some people do not have symptoms. Symptoms may be mild.They can include:
- Diarrhea or constipation
- Fatigue, lack of energy, or light-headedness when standing up or with exertion
- Loss of appetite
- Pale skin
- Problems concentrating
- Shortness of breath, mostly during exercise
- Swollen, red tongue or bleeding gums
- Confusion
- Depression
- Loss of balance
- Numbness and tingling in the hands and feet.
Exams and Tests
The doctor or nurse will perform a physical exam. Tests that may be done include:- Bone marrow examination (only needed if diagnosis is unclear)
- Complete blood count (CBC)
- Reticulocyte count
- Schilling test
- LDH
- Methylmalonic acid (MMA) level
- Vitamin B12 level
Pernicious anemia may also affect the results of the following tests:
Treatment
The goal of treatment is to increase your vitamin B12 levels.- Treatment involves a shot of vitamin B12 once a month. Persons with severely low levels of B12 may need more shots in the beginning.
- Some patients may also need to take vitamin B12 supplements by mouth. For some people, high-dose vitamin B12 tablets taken by mouth work well, and shots are not needed.
- A certain type of vitamin B12 may be given through the nose.
- Peripheral smear
- TIBC
8)Sickle Cell Anemia=
Sickle cell anemia is a disease passed down through families. The red blood cells which are normally shaped like a disc take on a sickle or crescent shape. Red blood cells carry oxygen to the body.Causes
Sickle cell anemia is caused by an abnormal type of hemoglobin called hemoglobin S. Hemoglobin is a protein inside red blood cells that carries oxygen.- Hemoglobin S changes the red blood cells. The red blood cells become fragile and shaped like crescents or sickles.
- The abnormal cells deliver less oxygen to the body's tissues.
- They can also easily get stuck in small blood vessels and break into pieces. This can interrupt healthy blood flow and cut down even more on the amount of oxygen flowing to body tissues.
Sickle cell disease is much more common in people of African and Mediterranean descent. It is also seen in people from South and Central America, the Caribbean, and the Middle East.
Symptoms
Symptoms usually do not occur until after the age of 4 months.Almost all people with sickle cell anemia have painful episodes called crises. These can last from hours to days. Crises can cause pain in the lower back, leg, joints, and chest.
Some people have one episode every few years. Others have many episodes each year. The crises can be severe enough to require a hospital stay.
When the anemia becomes more severe, symptoms may include:
Younger children with sickle cell anemia have attacks of abdominal pain.
The following symptoms may occur because small blood vessels become blocked by the abnormal cells:
- Painful and prolonged erection (priapism)
- Poor eyesight or blindness
- Problems with thinking or confusion caused by small strokes
- Ulcers on the lower legs (in adolescents and adults)
- Bone infection (osteomyelitis)
- Gallbladder infection (cholecystitis)
- Lung infection (pneumonia)
- Urinary tract infection
- Delayed growth and puberty
- Painful joints caused by arthritis.
Exams and Tests
Tests commonly performed to diagnose and monitor patients with sickle cell anemia include:- Bilirubin
- Blood oxygen saturation
- Complete blood count (CBC)
- Hemoglobin electrophoresis
- Serum creatinine
- Serum potassium
- Sickle cell test
Treatment
The goal of treatment is to manage and control symptoms, and to limit the number of crises. People with sickle cell disease need ongoing treatment, even when not having a crisis. It is best to get care from health care that take care of many patients with sickle cell anemia.People with this condition should take folic acid supplements. Folic acid helps make new red blood cells.
Treatment for a sickle cell crisis includes:
- Blood transfusions (may also be given regularly to prevent stroke)
- Pain medicines
- Plenty of fluids
- Hydroxyurea (Hydrea). Helps reduce the number of pain episodes (including chest pain and breathing problems) in some people
- Antibiotics. Help prevent bacterial infections, which are common in children with sickle cell disease
- Dialysis or kidney transplant for kidney disease
- Counseling for psychological complications
- Gallbladder removal in people with gallstone disease
- Hip replacement for avascular necrosis of the hip
- Surgery for eye problems
- Treatment for overuse or abuse of narcotic pain medicines
- Wound care for leg ulcers
People with sickle cell disease should have the following vaccinations to lower the risk of infection:
- Haemophilus influenzae vaccine (Hib)
- Pneumococcal conjugate vaccine (PCV)
- Pneumococcal polysaccharide vaccine (PPV)
9)Thalassemia=
Thalassemia is a blood disorder passed down through families (inherited) in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein in red blood cells that carries oxygen. The disorder results in large numbers of red blood cells being destroyed, which leads to anemia.Causes
Hemoglobin is made of two proteins: Alpha globin and beta globin. Thalassemia occurs when there is a defect in a gene that helps control production of one of these proteins.There are two main types of thalassemia:
- Alpha thalassemia occurs when a gene or genes related to the alpha globin protein are missing or changed (mutated).
- Beta thalassemia occurs when similar gene defects affect production of the beta globin protein.
Beta thalassemias occur most often in persons of Mediterranean origin. To a lesser extent, Chinese, other Asians, and African Americans can be affected.
There are many forms of thalassemia. Each type has many different subtypes. Both alpha and beta thalassemia include the following two forms:
- Thalassemia major
- Thalassemia minor
Thalassemia minor occurs if you receive the faulty gene from only one parent. Persons with this form of the disorder are carriers of the disease. Most of the time, they do not have symptoms.
Beta thalassemia major is also called Cooley's anemia.
Risk factors for thalassemia include:
- Asian, Chinese, Mediterranean, or African American ethnicity
- Family history of the disorder.
Symptoms
The most severe form of alpha thalassemia major causes stillbirth (death of the unborn baby during birth or the late stages of pregnancy).Children born with thalessemia major (Cooley's anemia) are normal at birth, but develop severe anemia during the first year of life.
Other symptoms can include:
- Bone deformities in the face
- Fatigue
- Growth failure
- Shortness of breath
- Yellow skin (jaundice)
Treatment
Treatment for thalassemia major often involves regular blood transfusions and folate supplements.If you receive blood transfusions, you should not take iron supplements. Doing so can cause a high amount of iron to build up in the body, which can be harmful.
Persons who receive a lot of blood transfusions need a treatment called chelation therapy. This is done to remove excess iron from the body.
A bone marrow transplant may help treat the disease in some patients, especially children.















No comments:
Post a Comment
Thank You.